Trichobezoars in pediatric surgery: a narrative review of clinical perspectives, surgical strategies, and psychological considerations
Introduction
Background
Bezoars are accumulations of undigested material forming mass-like structures within the digestive tract V体育官网入口. Although they primarily occur in the stomach, they can be found anywhere from the oesophagus to the rectum.
The term “bezoar” comes from the Persian “panzehr” and Arabic “badzehr”, both meaning “antidote” VSports在线直播. Until the 18th century, they were believed to have magical properties and were used as antidotes and talismans (1-3).
There are four main types of bezoars (4): phytobezoars, composed of plant fibers and tannins; trichobezoars, made up of hair and fibers, commonly linked to trichotillomania and trichophagia; lactobezoars, occurring in newborns due to milk concretions; and pharmacobezoars, resulting from medication ingestion. Other reported causes include antacids (5), candy, chewing gum (6,7) and paper (8) V体育2025版. Trichobezoars are relatively rare, accounting for approximately 6% of all bezoars.
They typically result from the repeated ingestion of hair (trichophagia), often linked to underlying psychiatric disorders such as trichotillomania. Since hair is resistant to digestion and gastric motility, it accumulates over time and may eventually form large, obstructive gastric masses VSports.
Rationale and knowledge gap
Although rare, pediatric trichobezoars present unique challenges that differ from those observed in adults VSports app下载. Children may have more subtle or delayed symptoms, and the psychological profile often necessitates a different diagnostic and therapeutic approach. In addition, there is currently no consensus on optimal management—particularly regarding the role of endoscopic removal versus surgery, and how to effectively prevent recurrence.
Psychological factors are central to this condition. Most pediatric patients with trichobezoars suffer from underlying psychiatric disorders such as trichotillomania and trichophagia. Ignoring these comorbidities increases the risk of recurrence, even after technically successful surgical treatment. Therefore, understanding the psychological dimension is essential for effective and lasting care V体育官网.
Objective (V体育ios版)
This article aims to synthesize current data on the diagnosis, management, and psychiatric aspects of trichobezoars in children. We present this article in accordance with the Narrative Review reporting checklist (available at https://pm.amegroups.com/article/view/10.21037/pm-25-41/rc).
Methods (VSports)
We searched for papers published without time restrictions on PubMed, Scopus, and Web of Science databases in November 2023, using the title and abstract keywords “trichobezoar”, “Rapunzel syndrome”, “gastric bezoars”, “surgical management of bezoars”, “endoscopic removal of bezoars”, and “trichotillomania”. Studies published in English and French were included in our review. Case reports, case series, retrospective and prospective cohort studies, systematic reviews, and meta-analyses discussing epidemiology, pathophysiology, clinical presentation, diagnosis, and management of trichobezoars were selected. Non-human studies, studies on other types of bezoars without mention of trichobezoars, and articles lacking sufficient clinical data were excluded. Additional references were identified through citation tracking of key articles. The selection of references was agreed upon by two independent reviewers, with disagreements resolved through discussion or consultation with a third reviewer. The search strategy is summarized in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 1st November, 2023 |
| Databases and other sources searched | PubMed, Scopus, and Web of Science |
| Search terms used | “Trichobezoar”, “Rapunzel syndrome”, “gastric bezoars”, “surgical management of bezoars”, “endoscopic removal of bezoars”, and “trichotillomania” |
| Timeframe | All published articles were included without time restrictions |
| Inclusion and exclusion criteria | Inclusion: case reports, case series, retrospective and prospective cohort studies, systematic reviews, and meta-analyses discussing epidemiology, pathophysiology, clinical presentation, diagnosis, and management strategies for trichobezoars |
| Exclusion: non-human studies, studies focusing on other types of bezoars without mention of trichobezoars, and articles lacking sufficient clinical data | |
| Selection process | Title and abstract screening: conducted by two independent reviewers |
Pathophysiology (V体育平台登录)
In adults, bezoar formation is associated with conditions such as cystic fibrosis, diabetes, hypothyroidism, renal failure, and gastric motility disorders (7). Psychiatric disorders, particularly in patients with gastroparesis or a history of gastric surgery (resections, bypass, bariatric procedures), also increase susceptibility (9).
In children, bezoars are often linked to pica, a condition characterized by ingestion of non-nutritive substances (10). Trichobezoars are more frequent in adolescent females with trichotillomania, a compulsive hair-pulling disorder often concealed due to fear of parental reprimand, leading to trichophagia, pulled hair ingestion (11).
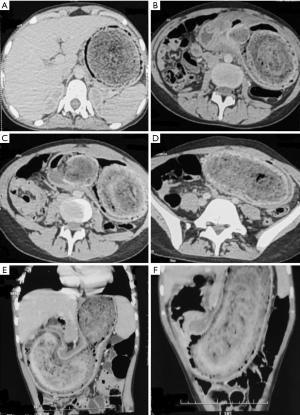
Once ingested, hair and fibers become trapped within the gastric folds, disrupting normal peristalsis. Lipid and mucus deposits contribute to the formation of a smooth, glistening mass, often causing halitosis. Gastric acid exposure denatures the hair, giving it a blackish color regardless of its original shade (12). Over time, the mass molds to the shape of the stomach (Figure 1) and may extend beyond the pylorus into the duodenum or small intestine (13), leading to Rapunzel syndrome, first described by Vaughan in 1968 (14). This can cause intestinal obstruction, intussusception, pancreatitis, or cholestatic jaundice due to ampullary obstruction. Detached fragments may migrate distally, resulting in small bowel obstruction.
V体育官网入口 - Epidemiology
Trichobezoars predominantly affect the pediatric population, with up to 90% of cases occurring in females younger than 20 years (15). However, rare cases in younger children and males have also been described, suggesting the need for high clinical suspicion across age and gender groups (10).
Clinical presentation and complications
Trichobezoars are diagnosed incidentally, through classic symptoms, or after complications arise—especially in Rapunzel syndrome cases. They can be mistaken for tuberculosis (16) or cancer.
Initially, trichobezoars may be asymptomatic. Over time, they can cause abdominal pain, distension, intermittent constipation, and vomiting (17). If left undiagnosed, they may lead to severe malnutrition, early satiety, weight loss, and fatigue (18-20). Halitosis is a common finding, often indicative of gastric content decomposition. Some patients may also pass hair in their stools (16).
On physical examination, a firm, non-tender epigastric mass is frequently detected. While not always present, alopecia or hair thinning should raise suspicion (21). A history of trichophagia is a crucial diagnostic clue, particularly in adolescent females (11). Additionally, some reports link trichobezoars to autism spectrum disorder (22,23).
Trichobezoars are strongly associated with psychiatric disorders, particularly trichotillomania and trichophagia. Trichotillomania is typically divided into two subtypes: the focused type, where hair-pulling is a conscious response to stress, and the automatic type, which occurs unconsciously (24). Many children diagnosed with trichobezoars also exhibit other psychological conditions, such as pica, attention deficit hyperactivity disorder (25), intellectual disabilities (26), or a history of emotional trauma (27). These overlapping disorders complicate diagnosis and emphasize the need for thorough psychiatric evaluation. Moreover, neurobiological studies suggest dysregulation in corticostriatal circuits in patients with trichotillomania, providing a rationale for integrating both behavioral and pharmacological interventions (28).
Complications can be serious in Rapunzel syndrome, where the trichobezoar extends past the pylorus and causes intestinal blockage, bilious vomiting, and absence of stool or gas (29). Gastric perforation, though rare, may present as an acute abdomen (30) but can also remain asymptomatic if it occurs in the posterior stomach wall, isolated by the bezoar mass (31). Other reported complications include intussusception due to migrating bezoar fragments (32,33), gastrointestinal bleeding from pressure-induced mucosal ulceration (34), and dysphagia when the bezoar obstructs the gastroesophageal junction (35). Bezoars extending into the duodenum can also cause pancreatitis (36-38) or jaundice (39) by obstructing the ampulla of Vater. Metabolic disturbances related to malnutrition may lead to electrolyte imbalances and neurological symptoms such as seizures or encephalopathy (16). Additionally, rare cases of generalized edema (40), amenorrhea, and cerebral venous thrombosis have been reported in the literature (19).
Diagnostic workup
The diagnosis of trichobezoars requires a thorough clinical evaluation supported by imaging and laboratory investigations.
Traditionally, bezoars were identified on plain radiographs as a mottled intragastric mass conforming to the stomach’s contours, with a radiolucent rim and possible displacement of the transverse colon. A speckled gas pattern or an intragastric filling defect may also be seen. However, plain radiographs alone diagnose only 18% of cases, limiting their reliability (41).
Contrast-enhanced upper abdominal radiographs confirm that a mobile irregular, coherent intraluminal mass is present. The mass is best visualized on delayed films after most of the barium has left the stomach or following the introduction of air into the stomach to produce a double contrast effect (41). Calcified tumors and fecalomas, which can sometimes mimic the appearance of trichobezoars, are also easily recognizable on a plain abdominal radiograph (41,42).
Ultrasound, frequently the first-line imaging modality due to its accessibility and safety, typically shows a well-defined hyperechoic mass with posterior acoustic shadowing. Point-of-care ultrasound (POCUS) has proven useful for rapid diagnosis (43), distinguishing trichobezoars from food-filled stomachs via a clear, intense acoustic shadow behind an anterior band of echogenicity (44). In some cases, a ‘twinkling’ artifact may also be observed, as noted in one case from a multicenter series on pediatric trichobezoars, caused by the rough surface of tightly packed hair (45). Additionally, ultrasound aids in differentiating trichobezoars from other epigastric masses, such as pancreatic pseudocysts, neuroblastomas, or gastric duplications, which have distinct sonographic appearances.
However, computed tomography (CT) remains the gold standard for diagnosing trichobezoars (31). As first described by Newman in 1988 (44), the characteristic CT appearance is an intragastric mass made of compressed concentric rings with entrapped air and debris (46) (Figure 2). CT also helps determine the extension of the bezoar into the duodenum (Rapunzel syndrome), locate any detached fragments that may have migrated into the small intestine, and assess for complications such as reactive gastritis (manifested as wall thickening with mucosal enhancement), obstruction, perforation, or intussusception (47).
Upper gastrointestinal endoscopy serves as both a diagnostic and therapeutic tool. It allows direct visualization of the trichobezoar, confirming its size and consistency. Endoscopy is particularly useful when other imaging modalities yield inconclusive results or when small bezoars are suspected.
Laboratory studies may reveal anemia (48), electrolyte imbalances, or hypoalbuminemia due to malnutrition or chronic blood loss (18), particularly in complicated cases. Indeed, iron deficiency anemia may arise from occult gastrointestinal bleeding secondary to mucosal ulceration.
"VSports在线直播" Management
Management of trichobezoar involves a combination of medical, endoscopic, and surgical approaches depending on the size, location, and severity of complications. Additionally, addressing underlying psychological disorders such as trichotillomania and trichophagia is essential to prevent recurrence.
Endoscopic management
For small trichobezoars confined to the stomach without associated complications, non-invasive strategies can be effective. Endoscopic removal is the preferred first-line treatment because enzymatic dissolution [e.g., papain, cellulase, or Coca-Cola (49,50)], effective in other bezoars, is ineffective against hair due to its resilient structure. Endoscopic removal is also possible for trichobezoars with an elongated shape, with intravenous glucagon administration facilitating relaxation of the lower oesophageal sphincter, as described by Saeed et al. (51). Larger trichobezoars, however, often require fragmentation for complete extraction. Tools such as biopsy forceps, snares, endoscopic scissors (52), and variceal ligator caps (53) have been employed with mixed results. Other fragmentation methods, such as lasers, water jets (54), and extracorporeal shock-wave lithotripsy have also been investigated but proven ineffective (55). Electrical devices may be considered as alternatives. However, these tools may cause mucosal injury or perforation, particularly when synthetic fibers release hydrogen chloride (56).
While early studies reported success rates as low as 5% (38), advancements in endoscopic techniques have led to improved outcomes, with success rates now reaching approximately 30% (56). However, the therapeutic efficacy of endoscopy remains largely confined to smaller trichobezoars. Larger masses tend to be refractory to endoscopic extraction due to their size, density, and the difficulty of achieving complete fragmentation and removal. Moreover, endoscopic fragmentation may lead to distal migration of bezoar fragments, potentially resulting in small-bowel obstruction (57).
Surgical management (VSports)
Surgical treatment remains the most effective and definitive approach. The optimal approach for trichobezoar removal remains controversial. While laparotomy remains the gold standard for large or complicated trichobezoars (58), laparoscopy offers significant advantages in terms of recovery and postoperative outcomes, particularly in less complicated cases.
Laparotomy with gastrotomy provides direct access to the bezoar and facilitates complete removal, including any fragments in the intestines. However, it is associated with greater postoperative morbidity, including pain, prolonged hospitalization, and infection risks. To mitigate these risks, some surgeons advocate for wound protectors (59) or seromuscular suturing of the stomach to the skin incision (60).
Since Nirasawa’s (61) first laparoscopic trichobezoar extraction in 1998, various refinements have been reported to optimize the procedure. Laparoscopic removal poses two main challenges: minimizing contamination during stomach access and avoiding a large incision that negates the benefits of minimally invasive surgery.
Early techniques for trichobezoar access, such as Nirasawa’s (61), involved a large anterior gastrotomy, increasing the risk of peritoneal contamination. To mitigate this, Ulukent (62) proposed enclosing the bezoar in an endobag inside the stomach before extraction. Dorn (63) introduced a laparoscopic method using a small gastrotomy with a blunt trocar, deploying a gastric balloon to stabilize the intragastric port, followed by carbon dioxide insufflation and fragmentation via a working trocar. Kanetaka et al. (64) described a combined laparoscopic-endoscopic approach, using a mini-laparotomy in the epigastric region for gastrotomy and inserting a 5 mm laparoscopic port for fragmentation with laparoscopic scissors. Filipi (65) proposed an alternative using two modified percutaneous endoscopic gastrostomy (PEG) ports for laparoscopic fragmentation. Though these approaches avoid large incisions, they remain technically demanding and time-consuming. Song et al. (66) emphasized the difficulty of fragmenting large or dense bezoars with laparoscopic scissors.
Once freed, trichobezoar extraction remains technically challenging. Various methods have been proposed, including suprapubic incisions, mini-laparotomy extensions via the left lower quadrant trocar incision, and upper midline incisions (61,67,68). While these approaches allow for intact removal, they are associated with an increased risk of wound infection (67). To minimize complications, Cintolo et al. and Fraser et al. (69,70) suggested extracting the bezoar in a controlled manner by bringing the extraction bag’s neck through a trocar incision for piecemeal removal. Similarly, Dorne (63) utilized a working scope to extract fragments. For exclusively intragastric fragmentation, Kanetaka and Filipi favored endoscopic removal (64,65).
Each surgical technique used in the treatment of trichobezoars has its own advantages and limitations (Table 2). The choice of surgical approach should be guided by the size and location of the bezoar, the presence of complications, and the surgeon’s expertise. While both laparotomy and laparoscopy are viable options for non-complicated cases, it is essential to exercise caution when considering a minimally invasive approach. Laparoscopy may be suitable for selected patients with small to moderate bezoars, but its application is generally limited in cases of large trichobezoars that require significant traction for removal. In such scenarios, the laparoscopic technique carries a higher risk of peritoneal contamination, prolonged operative time, and conversion to open surgery, potentially negating its minimally invasive benefits. Therefore, when the bezoar extends beyond the pylorus or is associated with complications, laparotomy remains the preferred approach to ensure safe and complete extraction.
Table 2
| Surgical method | Advantages | Disadvantages | Indications |
|---|---|---|---|
| Laparotomy | • Ensures complete bezoar extraction | • Higher morbidity | • Large trichobezoars (>10 cm) |
| • Lower recurrence risk | • Longer recovery time | • Presence of complications | |
| • Increased risk of wound infection | |||
| Laparoscopy | • Minimally invasive | • Technically challenging | • Moderate-sized bezoars (5–10 cm) |
| • Reduced postoperative pain | • Prolonged operative time | • No significant complications | |
| • Lower risk of wound infection | • Risk of peritoneal contamination | ||
| • Better cosmetic outcome | |||
| Hybrid approach (laparoscopy + endoscopy) | • Combines advantages of both techniques |
• Requires advanced expertise | • Cases where endoscopic assistance can facilitate extraction |
| • Improved visualization | • Prolonged surgical time | • Bezoars that require fragmentation but can be managed with minimal invasive surgery | |
| • Allows controlled fragmentation and extraction |
• Risk of incomplete removal if not well-coordinated | ||
| • Minimizes peritoneal contamination risk |
Some authors advocate for a temporary gastrostomy tube (7–10 days) to facilitate gastric decompression and restore normal peristalsis, particularly in cases of prolonged gastric distension (31).
Psychiatric interventions
Psychiatric intervention is essential in the management of trichobezoars, not only to prevent recurrence but to address underlying psychiatric conditions. Cognitive-behavioral therapy (CBT), particularly habit reversal training (HRT), remains the most evidence-based first-line intervention (10,71). HRT assists patients in identifying triggers and adopting alternative behaviors. Also, new technologies, such as wearable behavioral devices that detect hand movement toward the scalp, have shown promise in supporting HRT adherence in children (72). Emerging modalities, such as dialectical behavior therapy (DBT) and acceptance and commitment therapy (ACT), have shown efficacy in patients with comorbid emotional dysregulation and obsessive-compulsive features (73). Despite these advancements, relapse remains common, especially when follow-up is unstructured or prematurely discontinued. Relapse rates may reach 50–67% in the absence of ongoing psychiatric support (73,74).
Pharmacological options, such as selective serotonin reuptake inhibitors (SSRIs), glutamate modulators, and atypical antipsychotics, may be beneficial in moderate to severe cases. Notably, N-acetylcysteine (NAC) has shown promise in adults with trichotillomania and has good tolerability in pediatric patients, though its efficacy may be limited in those with automatic hair-pulling behaviors (72). However, the role of medication remains controversial in pediatric populations, with limited and variable evidence (28,72). Some patients may require combined or sequential therapies to achieve lasting results.
Recurrence after surgery is frequently reported in the absence of psychiatric care, emphasizing the need for multidisciplinary management. Ideal care involves pediatric surgeons, psychiatrists, pediatricians, child psychologists, and, when possible, school-based counselors to ensure behavioral continuity in everyday environments (27). Parental education and involvement are essential in monitoring signs of relapse, promoting adherence to treatment, and reducing stigma (75). A minimum psychiatric follow-up of 12 months postoperatively is recommended to optimize long-term outcomes (73).
Limitations
This review is limited by the predominance of case reports and small case series in the available literature, which may reduce generalizability. Future prospective studies comparing surgical techniques and psychiatric interventions are needed.
Conclusions (V体育平台登录)
Trichobezoars present significant challenges in pediatric surgery, with ongoing controversies regarding the optimal surgical approach. Although laparotomy remains the gold standard for large or complicated cases, laparoscopic and hybrid techniques provide minimally invasive alternatives. However, their efficacy remains debated due to technical challenges. The high recurrence rate due to underlying psychiatric disorders highlights the need for a multidisciplinary approach. Future research should focus on comparative studies of surgical techniques, advancements in minimally invasive removal methods, long-term psychiatric management strategies, and early screening tools to prevent recurrence and improve patient outcomes.
"VSports最新版本" Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://pm.amegroups.com/article/view/10.21037/pm-25-41/rc
Peer Review File: Available at https://pm.amegroups.com/article/view/10.21037/pm-25-41/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://pm.amegroups.com/article/view/10.21037/pm-25-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Williams RS. The fascinating history of bezoars. Med J Aust 1986;145:613-4.
- Eng K, Kay M. Gastrointestinal bezoars: history and current treatment paradigms. Gastroenterol Hepatol (N Y) 2012;8:776-8.
- DeBakey M, Ochsner A. Bezoars and concretions: A comprehensive review of the literature with an analysis of 303 collected cases and a presentation of 8 additional cases. Surgery 1939;5:132-60.
- Dorterler ME, Günendi T, Çakmak M, et al. Bezoar types in children and aetiological factors affecting bezoar formation: A single-centre retrospective study. Afr J Paediatr Surg 2023;20:8-11. ["V体育平台登录" Crossref] [PubMed]
- Kaplan M, Ozeri Y, Agranat A, et al. Antacid bezoar in a premature infant. Am J Perinatol 1995;12:98-9. [Crossref] [PubMed]
- Yulevich A, Finaly R, Mares AJ. Candy bezoar: an unusual cause of food bolus bezoar. J Pediatr Gastroenterol Nutr 1993;17:108-10.
- Milov DE, Andres JM, Erhart NA, et al. Chewing gum bezoars of the gastrointestinal tract. Pediatrics 1998;102:e22. [Crossref] [PubMed]
- Majeski JA. Paper bezoar in the stomach. South Med J 1985;78:1520. ["V体育官网" Crossref] [PubMed]
- Escamilla C, Robles-Campos R, Parrilla-Paricio P, et al. Intestinal obstruction and bezoars. J Am Coll Surg 1994;179:285-8.
- Ahmed M, Habib M, Memon H, et al. Trichotillomania, Trichophagia and Trichobezoar in a Male Paediatric Patient: A Case Report and Literature Review. Int J Surg Case Rep 2024;117:109520. [Crossref] [PubMed]
- Sehgal VN, Srivastava G. Trichotillomania +/- trichobezoar: revisited. J Eur Acad Dermatol Venereol 2006;20:911-5. [Crossref] [PubMed]
- Friedlander FC, Kushlick P. Trichobezoar. Arch Dis Child 1954;29:556-60. [Crossref] [PubMed]
- Sood AK, Bahl L, Kaushal RK, et al. Childhood trichobezoar. Indian J Pediatr 2000;67:390-1. [V体育平台登录 - Crossref] [PubMed]
- Vaughan ED Jr, Sawyers JL, Scott HW Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery 1968;63:339-43.
- Lee J. Bezoars and foreign bodies of the stomach. Gastrointest Endosc Clin N Am 1996;6:605-19.
- Mirza MB, Talat N, Saleem M. Gastrointestinal trichobezoar: An experience with 17 cases. J Pediatr Surg 2020;55:2504-9. [Crossref] [PubMed]
- Hurwitz S, McAlenney PF. Trichobezoar in children; review of the literature and report of two cases. AMA Am J Dis Child 1951;81:753-61.
- Patel TP, Ahmed M, Ahmed Z, et al. Trichobezoar causing malnutrition. International Journal of Contemporary Pediatrics 2022;9:396-8.
- Shastri M, Raval DM, Rathod VM, et al. A Triad of Trichobezoar: Rapunzel Syndrome, Severe Malnutrition, and Cerebral Venous Thrombosis. Cureus 2023;15:e38016. [Crossref] [PubMed]
- Sanders MK. Bezoars: From Mystical Charms to Medical and Nutritional Management. Practical Gastroenterology 2004;28:37-50.
- Yik YI, How AK A. ‘Hairy’ problem: Trichotillomania, trichophagia and trichobezoars. Singapore Med J 2016;57:411. [Crossref] [PubMed]
- Serour F, Witzling M, Frenkel-Laufer D, et al. Intestinal obstruction in an autistic adolescent. Pediatr Emerg Care 2008;24:688-90. [Crossref] [PubMed]
- Wijetilleke A, Sakran M, Kamat-Nerikar R. Vomiting in a girl with autism. Clin Pediatr (Phila) 2009;48:224-7. [Crossref] [PubMed]
- Grant JE, Chamberlain SR. Automatic and focused hair pulling in trichotillomania: Valid and useful subtypes? Psychiatry Res 2021;306:114269. [Crossref] [PubMed]
- Forooghi M, Shahrokhi R, Yousufzai S. A giant trichobezoar in a child with attention deficit hyperactivity disorder: A case report. Int J Surg Case Rep 2024;123:110283. [Crossref] [PubMed]
- Roy D. EPA-0270 – Trichotillomania and other co-morbdity in intellectually disabled children. two case studies. European Psychiatry 2014;29:1.
- Kumar VS, Shenoy AM. Trichobezoars in children - A psychological perspective. Asian J Psychiatr 2024;101:104217. [V体育官网入口 - Crossref] [PubMed]
- Snorrason I, Ricketts EJ, Stein AT, et al. Sex Differences in Age at Onset and Presentation of Trichotillomania and Trichobezoar: A 120-Year Systematic Review of Cases. Child Psychiatry Hum Dev 2022;53:165-71. [Crossref] [PubMed]
- Hassan AA, Panesar KJ. The Rapunzel syndrome: a rare presentation of trichobezoar. Ulster Med J 1989;58:94-6.
- Marique L, Wirtz M, Henkens A, et al. Gastric Perforation due to Giant Trichobezoar in a 13-Year-Old Child. J Gastrointest Surg 2017;21:1093-4. [Crossref (V体育官网)] [PubMed]
- Gupta A, Mittal D, Srinivas M. Gastric Trichobezoars in Children: Surgical Overview. Int J Trichology 2017;9:50-3. ["VSports注册入口" Crossref] [PubMed]
- Dalshaug GB, Wainer S, Hollaar GL. The Rapunzel syndrome (trichobezoar) causing atypical intussusception in a child: a case report. J Pediatr Surg 1999;34:479-80. [Crossref] [PubMed]
- Won MM, Sacks MA, Leigh R, et al. An Unusual Case of Primary Ileal Trichobezoar Causing Intussusception. Am J Case Rep 2022;23:e935460. [Crossref] [PubMed]
- Harrabi F, Ammar H, Ben Latifa M, et al. Gastric Trichobezoar Causing Gastrointestinal Bleeding: A Case Report. Cureus 2022;14:e30282. [Crossref] [PubMed]
- Klink CD, Jansen M, Schumpelick V. Dysphagia of unknown cause in a young female. Chirurg 2008;79:1162-4. [V体育官网 - Crossref] [PubMed]
- Abourazzak S, Jerrar IO, Lakhdar Idrissi M, et al. Rapunzel syndrome complicated with pancreatitis, intussusception and intestinal perforation. BMJ Case Rep 2022;15:e247005. [V体育官网入口 - Crossref] [PubMed]
- AlQaseer A, AlHarmi RAR, AbuAli N, et al. Rare case of trichobezoar causing pancreatitis in a young woman. BMJ Case Rep 2019;12:e229173. [V体育官网 - Crossref] [PubMed]
- Gorter RR, Kneepkens CM, Mattens EC, et al. Management of trichobezoar: case report and literature review. Pediatr Surg Int 2010;26:457-63. [Crossref] [PubMed]
- Verma A, Sharma S, Tyagi G, et al. Huge trichobezoar causing obstructive jaundice. BMJ Case Rep 2014;2014:bcr2013201667. [Crossref] [PubMed]
- Nour I, Abd Alatef M, Megahed A, et al. Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health 2019;39:76-8. [Crossref] [PubMed]
- Ripollés T, García-Aguayo J, Martínez MJ, et al. Gastrointestinal bezoars: sonographic and CT characteristics. AJR Am J Roentgenol 2001;177:65-9. [Crossref] [PubMed]
- Delabrousse E, Lubrano J, Sailley N, et al. Small-bowel bezoar versus small-bowel feces: CT evaluation. AJR Am J Roentgenol 2008;191:1465-8. [Crossref] [PubMed]
- Chiang E, Balasubramanian S, Rabiner JE. Point-of-Care Ultrasound of a Pediatric Gastric Trichobezoar: A Case Report. Pediatr Emerg Care 2023;39:892-4. [Crossref] [PubMed]
- Newman B, Girdany BR. Gastric trichobezoars--sonographic and computed tomographic appearance. Pediatr Radiol 1990;20:526-7. [Crossref] [PubMed]
- Shah RD, Grither A, Cohen SG, et al. Hair Today, OR Tomorrow: A Multicenter Case Series of Gastric Bezoars in Children Diagnosed With Point-of-Care Ultrasound. Pediatr Emerg Care 2025;41:63-7. [Crossref] [PubMed]
- Tamminen J, Rosenfeld D. CT diagnosis of a gastric trichobezoar. Comput Med Imaging Graph 1988;12:339-41. [V体育官网 - Crossref] [PubMed]
- Kyin C, Patel P, Casas-Melley A, et al. Acute Case of Trichobezoar Diagnosed From Computed Tomography and 3D Images: Rapunzel Syndrome Re-examined. Cureus 2023;15:e35597. [Crossref] [PubMed]
- Nissen M, Tröbs RB. Epigastric Mass-a 4-Year-Old With Trichobezoar and Anemia. Dtsch Arztebl Int 2022;119:252. [Crossref (V体育官网)] [PubMed]
- Matsuoka R, Masuda S, Fujita S, et al. Trichobezoar effectively treated with direct endoscopic injection of Coca-Cola: A case report. DEN Open 2023;4:e283. [Crossref] [PubMed]
- Gülerman F, Güven B, Demir S, et al. How should trichobezoar be treated in children? Turk J Gastroenterol 2019;30:660-1. [Crossref] [PubMed]
- Saeed ZA, Ramirez FC, Hepps KS, et al. A method for the endoscopic retrieval of trichobezoars. Gastrointest Endosc 1993;39:698-700. [V体育官网入口 - Crossref] [PubMed]
- Aybar A, Safta AM. Endoscopic removal of a gastric trichobezoar in a pediatric patient. Gastrointest Endosc 2011;74:435-7. [Crossref] [PubMed]
- Lu D, Berglund B, Xia Y, et al. Endoscopic removal of a massive trichobezoar in a pediatric patient by using a variceal ligator cap: A case report and literature review. Front Med (Lausanne) 2022;9:1020648. [Crossref] [PubMed]
- Kuo JY, Mo LR, Tsai CC, et al. Nonoperative treatment of gastric bezoars using electrohydraulic lithotripsy. Endoscopy 1999;31:386-8. [Crossref (V体育安卓版)] [PubMed]
- Van Gossum A, Delhaye M, Cremer M. Failure of non-surgical procedures to treat gastric trichobezoar. Endoscopy 1989;21:113. [Crossref] [PubMed]
- Niţă AF, Hill CJ, Lindley RM, et al. Human and Doll’s Hair in a Gastric Trichobezoar, Endoscopic Retrieval Hazards. J Pediatr Gastroenterol Nutr 2020;71:163-70. [Crossref (VSports手机版)] [PubMed]
- Fallon SC, Slater BJ, Larimer EL, et al. The surgical management of Rapunzel syndrome: a case series and literature review. J Pediatr Surg 2013;48:830-4. [Crossref] [PubMed]
- Castle SL, Zmora O, Papillon S, et al. Management of Complicated Gastric Bezoars in Children and Adolescents. Isr Med Assoc J 2015;17:541-4.
- Cundy TP, Brownlee EM, Goh DW, et al. Simplified technique for retrieval of large trichobezoars in children. BMJ Case Rep 2015;2015:bcr2015210472. [Crossref] [PubMed]
- Javed A, Agarwal AK. A modified minimally invasive technique for the surgical management of large trichobezoars. J Minim Access Surg 2013;9:42-4. [Crossref] [PubMed]
- Nirasawa Y, Mori T, Ito Y, et al. Laparoscopic removal of a large gastric trichobezoar. J Pediatr Surg 1998;33:663-5. [Crossref] [PubMed]
- Ulukent SC, Ozgun YM, Şahbaz NA. A modified technique for the laparoscopic management of large gastric bezoars. Saudi Med J 2016;37:1022-4. [Crossref] [PubMed]
- Dorn HF, Gillick JL, Stringel G. Laparoscopic intragastric removal of giant trichobezoar. JSLS 2010;14:259-62. [Crossref] [PubMed]
- Kanetaka K, Azuma T, Ito S, et al. Two-channel method for retrieval of gastric trichobezoar: report of a case. J Pediatr Surg 2003;38:e7. [Crossref] [PubMed]
- Filipi CJ, Perdikis G, Hinder RA, et al. An intraluminal surgical approach to the management of gastric bezoars. Surg Endosc 1995;9:831-3. [Crossref] [PubMed]
- Song KY, Choi BJ, Kim SN, et al. Laparoscopic removal of gastric bezoar. Surg Laparosc Endosc Percutan Tech 2007;17:42-4. [Crossref (V体育2025版)] [PubMed]
- Shami SB, Jararaa AA, Hamade A, et al. Laparoscopic removal of a huge gastric trichobezoar in a patient with trichotillomania. Surg Laparosc Endosc Percutan Tech 2007;17:197-200. [Crossref] [PubMed]
- Sharma D, Srivastava M, Babu R, et al. Laparoscopic treatment of gastric bezoar. JSLS 2010;14:263-7. [Crossref (VSports手机版)] [PubMed]
- Cintolo J, Telem DA, Divino CM, et al. Laparoscopic removal of a large gastric trichobezoar in a 4-year-old girl. JSLS 2009;13:608-11. [Crossref] [PubMed]
- Fraser JD, Leys CM, St Peter SD. Laparoscopic removal of a gastric trichobezoar in a pediatric patient. J Laparoendosc Adv Surg Tech A 2009;19:835-7. [Crossref] [PubMed]
- Okumuş HG, Akdemir D, Temeltürk RD, et al. Impulsivity in adolescent girls diagnosed with trichotillomania: an evaluation of clinical and neuropsychological characteristics. Eur Child Adolesc Psychiatry 2024;33:617-27. [V体育安卓版 - Crossref] [PubMed]
- Melo DF, Lima CDS, Piraccini BM, et al. Trichotillomania: What Do We Know So Far? Skin Appendage Disord 2022;8:1-7. [Crossref] [PubMed]
- Ezoddin N, Sobhanian P, Mousavi SA, et al. Management of Gastric Trichobezoar in Children: A Case Report and Literature Review. Journal of Pediatrics Review 2025;13:41-8.
- Wang L, Chen Y, Chen S, et al. Gastrointestinal trichobezoars in the pediatric population: a retrospective study. BMC Pediatr 2024;24:124. ["V体育官网" Crossref] [PubMed]
- Almouallem MM, Hanna M, Martini N, et al. Trichobezoar as an Unusual Cause for Iron Deficiency Anemia: A Rare Case Report. Clin Case Rep 2025;13:e70186. [V体育官网 - Crossref] [PubMed]
Cite this article as: Alami Hassani Z, Andaloussi S, Annattah S, Dalero O, El Madi A. Trichobezoars in pediatric surgery: a narrative review of clinical perspectives, surgical strategies, and psychological considerations. Pediatr Med 2025;8:20.


 "V体育2025版"
"V体育2025版"