A retrospective cohort study on the feasibility and safety of IONM for the external branch of the superior laryngeal nerve during gasless unilateral subclavian approach endoscopic hemithyroidectomy
Highlight box
Key findings
• The use of intraoperative neuromonitoring (IONM) technology to explore and preserve the external branch of the superior laryngeal nerve (EBSLN) during subclavian endoscopic thyroid surgery is safe and feasible.
What is known, and what is new?
• The EBSLN is an important structure that requires careful protection during thyroid surgery. The use of IONM technology has advanced the anatomical preservation of the EBSLN VSports在线直播. We developed a novel method of gasless endoscopic thyroidectomy using a subclavian approach that eradicates the complications related to carbon dioxide insufflation and avoids visibleneck scarring. This method is particularly suitable for unilateral thyroid cancer surgery.
• In this study, we used IONM technology to identify and preserve the EBSLN during subclavian endoscopic thyroid surgery, which is performed laterally. This approach allowed for a dissection in line with the nerve’s trajectory, thus avoiding direct conflict with its course. Additionally, the magnifying effect of the endoscope enabled better differentiation between nerves and vascular muscular bundles, while IONM can serve as a method for further confirmation of the nerve V体育2025版.
What is the implication, and what should change now?
• This study used IONM technology to preserve the EBSLN during subclavicular endoscopic thyroid surgery, resulting in a scarless neck appearance, enhancing the quality of life of patients, and achieving superior functional preservation VSports app下载. However, due to the relatively small cohort size of this study, further research with larger sample sizes needs to be conducted to comprehensively evaluate the anatomical subtypes of the EBSLN and functional parameters of the approach.
Introduction
In recent years, the evolution of thyroid surgery has been marked by a growing emphasis on functional preservation, extending beyond the recurrent laryngeal nerve (RLN) to include the external branch of the superior laryngeal nerve (EBSLN) V体育官网. The EBSLN, which is characterized by its delicate structure, variable anatomical course (1), and subtle post-injury symptoms, poses significant challenges for intraoperative identification, protection, and post-injury evaluation (2). Injury to this nerve, though often underdiagnosed, can lead to significant vocal morbidity, including reduced pitch range, projection, and vocal fatigue (3). Visual identification alone may lead to misinterpretation of the EBSLN as tendinous muscle fibers or non-neural tissue, thereby reducing the accuracy of EBSLN recognition (4). The clinical need for consistent EBSLN preservation is therefore substantial, particularly in endoscopic approaches where tactile feedback is limited (5).
The introduction of intraoperative neuromonitoring (IONM) has represented a major advance in neural protection during thyroid surgery. Initially standardized for RLN monitoring, IONM techniques have been progressively adapted and refined for EBSLN identification (6). Several studies have demonstrated that IONM can significantly improve EBSLN identification rates compared to visual dissection alone, particularly in cases where the nerve is obscured by vascular structures or has a deep anatomical course (7-9) VSports手机版. The application and feasibility of IONM in gasless subclavian endoscopic thyroid surgery, however, remain underexplored.
Our team has previously reported on the value of IONM in video-assisted thyroidectomy (10). Building on this experience, we developed a gasless subclavian approach for endoscopic hemithyroidectomy, which offers excellent cosmetic results and operational ergonomics (11). A critical next step was to integrate IONM into this approach specifically for EBSLN preservation—a technically demanding endeavor given the remote operating angle and tissue dissection plane. This study therefore aims to report on the feasibility and safety of using IONM for EBSLN identification and protection in gasless subclavian endoscopic thyroid surgery, addressing a relevant gap in the current literature and offering technical insights for surgeons adopting this approach. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-369/rc).
Methods
Study design and participants
This single-center, retrospective cohort study was conducted to evaluate the feasibility and safety of IONM for identifying and preserving the EBSLN during gasless unilateral subclavian approach endoscopic hemithyroidectomy. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of Sir Run Run Shaw Hospital, Medical School, Zhejiang University (No. 20245-1106), and the requirement for informed consent was waived due to the retrospective nature of the study.
All patients who underwent the unilateral thyroidectomy and central neck dissection using the subclavian approach in the department of Head and Neck Surgery, Sir Run Run Shaw Hospital, Medical School, Zhejiang University between October 2023 and June 2024 were considered for enrollment (Table 1). Given the exploratory nature of this technique and the lack of preliminary data for formal power calculation, a sample size estimation was not performed a priori. Instead, we aimed to include all eligible patients within the study period to maximize data availability for this initial feasibility assessment. Ultimately, 48 patients met the criteria and were included in the final analysis.
"V体育官网" Table 1
| Variables | Value |
|---|---|
| Age (years) | 35.4±10.4 [19–59] |
| Gender | |
| Male | 9 (18.7) |
| Female | 39 (81.3) |
| Tumor size (mm) | |
| PTC | 7.0±2.7 [3–16] |
| T stage | |
| pT1a | 43 (89.6) |
| pT1b | 5 (10.4) |
| N stage | |
| PN0 | 22 (45.8) |
| pN1a | 26 (54.2) |
Data are presented as n (%) or mean ± standard deviation [range]. N, node; PTC, papillary thyroid carcinoma; T, tumor.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (I) cytologically confirmed papillary thyroid carcinoma with a maximum tumor diameter ≤3 cm on preoperative ultrasound; (II) scheduled for gasless unilateral subclavian endoscopic hemithyroidectomy with central compartment lymph node dissection; (III) no clinical or ultrasonographic evidence of lateral cervical lymph node metastasis (cN0); (IV) the maximum diameter of the thyroid lobe was less than 6 cm; and (V) no previous history of neck surgery or radiation therapy.
Exclusion criteria were: (I) had preoperative evidence of primary tumor or lymph node invasion into adjacent structures (e.g., the trachea, esophagus, or larynx); (II) had a tumor located close to the entry point of the larynx of the RLN or cricothyroid muscle; (III) preoperative vocal cord paralysis or documented hoarseness; and/or (IV) a known history of keloid formation.
Assessment of feasibility and safety
The primary feasibility outcome was the successful identification rate of the EBSLN using IONM. Secondary feasibility outcomes included the mean time required for EBSLN dissection and the total operative time.
The primary safety outcome was the incidence of EBSLN injury, which was comprehensively determined based on postoperative voice changes such as difficulty in raising pitch and vocal fatigue. Other safety outcomes included the incidence of transient or permanent RLN palsy, hypoparathyroidism (defined as symptomatic hypocalcemia or a corrected serum calcium level <2.0 mmol/L requiring supplementation), surgical site infection, and conversion to open surgery.
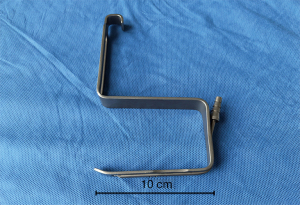
"V体育平台登录" Surgical instruments
The surgical instruments used in this study included standard endoscopic thyroid surgery instruments and custom-developed tools. More specifically, the instruments included: (I) a 30°, 10-mm diameter high-definition endoscope with a camera unit (KARL STORZ, Germany), endoscopic grasping forceps, endoscopic separating forceps, an endoscopy suction device, and a 36-cm ultrasonic scalpel (Johnson & Johnson, USA); and (II) custom-developed instruments, comprising a suspension hook with suction tubes (Figure 1). (III) IONM system: NIM-Response 3.0 (Medtronic, USA), used in intermittent mode to map the EBSLN.
Surgical methods
The patient was placed in a supine position with shoulder padding, and their head was slightly turned toward the healthy side. An anesthesia frame was fixed at the midpoint of the apex of the opposite axilla and shoulder to provide a cavity for suspension. An assistant holding the scope was sat at the patient’s head, and the primary surgeon was positioned at the patient’s feet. An instrument table and scrub nurse were also positioned at the patient’s head.
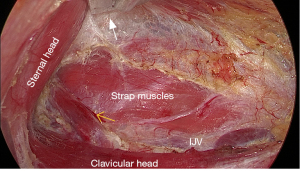
General anesthesia was induced with oral intubation with a nerve monitoring endotracheal tube. A skin incision was made along the inferior border of the clavicle, measuring approximately 3–3.5 cm, with the outer edge of the incision closely aligned with the inferior border of the clavicle. Surface markings were made for the posterior edge of the sternal head and the clavicular head of the sternocleidomastoid muscle (SCM), as well as the gap between them (Figure 2). The skin and subcutaneous tissue were incised along the predesigned incision, and the dissection was performed closely along the layer of the platysma toward the thyroid area to protect the branches of the supraclavicular nerves under direct vision.

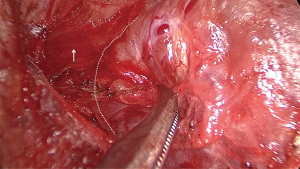
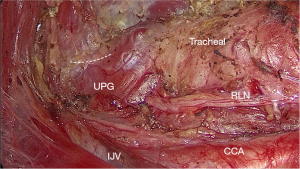
After the space between the sternal head and the clavicular head of the SCM was exposed, a specially designed suspension retractor was inserted and fixed to the anesthesia frame to elevate the skin flap (Figures 3,4). The dissection continued under the endoscope to separate the lateral edge of the strap muscles, and the suspension retractor was then placed beneath the strap muscles to lift the entire thyroid gland upward. The dissection was performed at the level of the inferior pole of the thyroid to locate and identify the RLN. The dissection proceeded upward along the nerve to the entry point into the larynx of the nerve.

Further dissection was performed on the tracheal side to cut off the Berry ligament and release the thyroid toward the opposite side. The tissue between the superior pole of the thyroid gland and the strap muscles was further dissected to expose the cricothyroid muscle. The dissection was performed laterally on the superior pole of the thyroid with intermittent 3 mA current stimulation to detect the EBSLN (12). A positive standard was based on electromyographic signals or the contraction of the entire cricothyroid muscle (13). Further exploration was performed along the area with the strongest electromyographic response, and upon locating a suspicious nerve, the current was adjusted to 1 mA for confirmation of the nerve (Figure 5).
After confirming the course of the nerve, further dissection was performed with an ultrasonic scalpel to coagulate the blood vessels of the superior pole of the thyroid. Next, the dissection was performed at the level of the inferior pole of the thyroid downward to the level of the brachiocephalic trunk to complete the central neck dissection. The resected specimens were carefully examined for any parathyroid glands and an immediate auto-transplantation was performed if any parathyroid gland was identified (14). The nerve was re-examined to confirm its function before the incision was closed.
Statistical analysis
Statistical analysis was performed using SPSS software version 29.0 (SPSS Inc., Armonk, NY, USA). Continuous variables with a normal distribution, such as operative time and patient age, are presented as mean ± standard deviation (SD) and were compared using independent samples t-tests. Continuous non-normally distributed data are presented as median with interquartile range (IQR). Categorical variables are presented as numbers and percentages (%). P value of less than 0.05 was considered statistically significant.
VSports最新版本 - Results
All patients underwent successful endoscopic surgery without conversion to open surgery. EBSLN dissection was performed in 46 of the 48 patients. In two of the patients no EBSLN dissection was completed, attempts were made to identify the nerve, the procedures took approximately 10 minutes each, but the nerve could not be located. To avoid potential damage from further manipulation, further exploration for the nerve was abandoned. Of the dissections, 25 were performed during left thyroidectomy and 23 were performed during right thyroidectomy. Additionally, 42 (87.5%) patients had positive electromyographic signals. Among the patients, 3 were classified as Cernea type 1, 41 as type 2a, and 2 as type 2b (15). Additionally, one patient had a nerve that ran deep to the inferior pharyngeal constrictor muscle (16) (Figure 6).
The mean operative time was 115.6±25.1 min (60–165 min). The mean dissection time was 3.4±1.0 mins (2–6 min). The mean tumor size was 7.0±2.7 mm (3–16 mm). The mean number of harvested central compartment lymph nodes was 9.1±4.4 (3–21). The mean number of lymph nodes with metastasis was 1.4±1.9 (0–9). The mean length of postoperative hospital stay was 2.9±0.7 days (2–5 days) (Table 2). Transient RLN injury occurred in 1 patient, who had recovered by the three-month follow up. No patients exhibited significant hoarseness or changes in pitch, and no permanent RLN palsy, permanent hypoparathyroidism, or incision infection occurred.
Table 2
| Variables | Value |
|---|---|
| Operative time (min) | 115.6±25.1 [60–165] |
| Time for dissection of the EBSLN (min) | 3.4±1.0 [2–6] |
| Dissected LNs | 9.1±4.4 [3–21] |
| LNs with metastasis | 1.4±1.9 [0–9] |
| Postoperative hospital stay (days) | 2.9±0.7 [2–5] |
| Classification of EBSLN | |
| Cernea 1 | 3 (6.3) |
| Cernea 2a | 41 (85.4) |
| Cernea 2b | 2 (4.2) |
| Complications | |
| Vocal cord palsy | |
| Transient | 1 (2.1) |
| Permanent | 0 |
Data are presented as number or mean ± standard deviation [range] or n (%). EBSLN, external branch of the superior laryngeal nerve; LN, lymph node.
Discussion
The superior laryngeal nerve is an important structure that requires careful protection during thyroid surgery. It originates from the vagus nerve ganglion and descends, branching into the internal and external branches at the level of the greater horn of the hyoid bone. The internal branch primarily contains visceral sensory fibers and innervates the mucosa above the vocal cords. The external branch (i.e., the EBSLN) mainly consists of special visceral motor fibers, innervating the muscles of swallowing and the cricothyroid muscle, which play a critical role in maintaining the tension of the vocal cords. The EBSLN is slender and exhibits a high degree of anatomical variability, making it susceptible to injury. Injury to this nerve often presents subtly with symptoms such as a low voice and vocal fatigue, unlike the obvious hoarseness that follows injury to the RLN. Moreover, the assessment of injury is challenging and may require procedures such as stroboscopic laryngoscopy or electromyography. In clinical practice, this nerve is often overlooked, with the literature reporting that the rate of injury to the EBSLN is 58% (17).
Traditional thyroid surgery has relied primarily on avoidance techniques to protect the EBSLN, such as ligating blood vessels close to the superior pole of the thyroid gland to keep them away from the nerve. While this can effectively protect nerves that are positioned further away from the superior pole of the thyroid gland or that run deep to the inferior pharyngeal constrictor muscle, it poses a high risk of injury to branches that run below or closely adjacent to the superior pole of the thyroid gland (18). In such cases, avoidance techniques carry significant uncertainty.
With advancements in surgical techniques and an increased emphasis on the importance of the superior laryngeal nerve, active exploration of the nerve has gained prominence (19). Approaches such as sternothyroid-hyoid triangle localization and the strap muscle interspace approach have been developed to enhance nerve protection (20,21). In recent years, intraoperative nerve monitoring technology and endoscopic techniques have significantly improved the ability of surgeons to not only assess but also actively explore and identify the anatomical course of the EBSLN during thyroidectomy. IONM in our study served as an active mapping tool to localize and trace the EBSLN’s route prior to dissection.
Satisfactory outcomes have been achieved by using a larger stimulation current (3 mA) in the sternothyroid-hyoid triangle and probing the area with the strongest muscular response, followed by a smaller current (1 mA) to confirm suspicious nerves. During this process, the twitching of the cricothyroid muscle and electromyography signals are used as positive indicators. The literature suggests that approximately 41–85% of EBSLNs have anastomotic connections with the RLN which can extend through the cricothyroid muscle sheath into the larynx, innervating the anterior one-third of the vocal cords, and exhibiting waveforms upon electrical stimulation (22). In this study, 42 patients presented with positive electromyography signals. If no waveform signals are detected, the overall twitching of the cricothyroid muscle can be considered a positive indicator. The magnifying effect of endoscopy optimizes the visualization of the EBSLN, facilitating its differentiation from surrounding muscular and fibrous structures. Our team has previously attempted to explore this nerve using nerve monitoring techniques in video-assisted thyroid surgery, the method has high practical value (10).
Since 2020, our team has been performing subclavicular endoscopic thyroid surgery and routine procedures such as unilateral thyroidectomy, total thyroidectomy, and lateral neck dissection (11,22,23). We aimed to dissect and protect the EBSLN during subclavicular endoscopic thyroid surgery. The course of most EBSLNs runs medial to the superior pole of the thyroid gland. The subclavicular endoscopic approach is performed laterally, allowing for a dissection direction that is in line with the nerve’s trajectory, and thus avoiding direct conflict with its course (24). This reduces the risk of dissection injury and minimizes excessive retraction or the flipping of the thyroid gland, which is particularly advantageous in protecting both the RLN and the EBSLN.
During EBSLN exploration, the exposure of the cricothyroid muscle serves as a confirmation marker. However, in the subclavicular approach, we often use retractors to lift the strap muscle, using the adhesions between the thyroid and strap muscle to pull the thyroid and the lateral central compartment specimen upward symmetrically. If the tissue between the thyroid and strap muscle is separated too early, the thyroid gland may sag downward and hinder the operation, increasing the difficulty of lateral dissection, especially at the entry point into the larynx.
On the basis of our experience, we adopted a segmented approach in this study, first exploring and isolating the RLN at the level of the inferior pole of the thyroid, and then proceeding upward along the nerve to the entry point into the larynx. After completing the dissection in this area, we cut off the Berry ligament from the tracheal side, isolating the tissue between the thyroid and trachea and initially exposing the cricothyroid muscle. We subsequently separated the tissue between the superior pole of the thyroid and the strap muscle to further expose the cricothyroid muscle and increase visibility in the superior pole region. The retractor position was adjusted as necessary to increase exposure in this area. We used larger electrical currents (3 mA) for stimulation in the lateral region of the superior pole of the thyroid, and along the area of the strongest muscular response, we further explored and confirmed the presence of the nerve using smaller currents (1 mA).
After the location of the EBSLN was confirmed, we followed its course slightly upward for further dissection and confirmed that the nerve was safely distanced before using an ultrasonic scalpel to coagulate the blood vessels at the superior pole of the thyroid. We were cautious to avoid injuring the swallowing muscles and the cricothyroid muscle. In one patient, despite repeated exploration in the area of the superior pole, the nerve tissue could not be clearly identified; however, twitching of the cricothyroid muscle was detected at 3mA current over the surface of the inferior pharyngeal constrictor muscle, and further exploration revealed the deep branch of the muscle, which was considered a nerve running deep to the inferior pharyngeal constrictor muscle (15,25).
In open and other endoscopic surgical approaches, the area around the superior pole of the thyroid is the most distant and narrow space, which inherently limits visualization during surgical operations. In our study, the use of a 10-mm 30° endoscope, combined with adjustments to the position of the retractor and appropriate rotation of the camera, provided sufficient visualization of the superior pole region and simplified the surgical procedure under adequate exposure. The magnifying effect of the endoscope further enabled better differentiation between nerves and vascular muscular bundles, facilitating the identification and confirmation of the EBSLN.
Conclusions
In our study, we attempted to isolate the EBSLN in 48 patients, successfully identified it in 46 patients, and identified one patient with a nerve that ran deep to the inferior pharyngeal constrictor muscle; thus, good exploration and protection of the EBSLN was achieved in this study. Due to the growth of operational dexterity, the time taken for isolation stabilized at approximately 3 minutes, and there was no significant increase in the surgical duration. The use of IONM technology to explore and preserve the EBSLN during subclavian endoscopic thyroid surgery is safe and feasible, suggesting its potential clinical application. However, the number of patients in this study was relatively small; thus, further research needs to be conducted to validate the efficacy and applicability of this method in the treatment of thyroid cancer.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-369/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-369/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-369/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-369/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of Sir Run Run Shaw Hospital, Medical School, Zhejiang University (No. 20245-1106) and the requirement for informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
"VSports手机版" References
- Erfan S, Saha S, Guha R, et al. Varying Course of External Branch of Superior Laryngeal Nerve (EBSLN) and Recurrent Laryngeal Nerve (RLN) in Thyroidectomy-An Observational Study. Indian J Otolaryngol Head Neck Surg 2024;76:1959-64. [Crossref] [PubMed]
- Zhao Y, Zhao Z, Zhang D, et al. Improving classification of the external branch of the superior laryngeal nerve with neural monitoring: a research appraisal and narrative review. Gland Surg 2021;10:2847-60. [V体育安卓版 - Crossref] [PubMed]
- Potenza AS, Araujo Filho VJF, Cernea CR. Injury of the external branch of the superior laryngeal nerve in thyroid surgery. Gland Surg 2017;6:552-62. ["VSports在线直播" Crossref] [PubMed]
- Barczyński M, Konturek A, Stopa M, et al. Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg 2012;36:1340-7. [Crossref] [PubMed]
- Uludag M, Aygun N, Kartal K, et al. Contribution of intraoperative neural monitoring to preservation of the external branch of the superior laryngeal nerve: a randomized prospective clinical trial. Langenbecks Arch Surg 2017;402:965-76. [Crossref] [PubMed]
- Cheruiyot I, Kipkorir V, Henry BM, et al. Surgical anatomy of the external branch of the superior laryngeal nerve: a systematic review and meta-analysis. Langenbecks Arch Surg 2018;403:811-23. [Crossref] [PubMed]
- Sanabria A, Kowalski LP, Nixon I, et al. Methodological Quality of Systematic Reviews of Intraoperative Neuromonitoring in Thyroidectomy: A Systematic Review. JAMA Otolaryngol Head Neck Surg 2019;145:563-73. [Crossref] [PubMed]
- Naytah M, Ibrahim I, da Silva S. Importance of incorporating intraoperative neuromonitoring of the external branch of the superior laryngeal nerve in thyroidectomy: A review and meta-analysis study. Head Neck 2019;41:2034-41. [Crossref] [PubMed]
- Uludag M, Yazici P, Aygun N, et al. A Closer Look at the Recurrent Laryngeal Nerve Focusing on Branches & Diameters: A Prospective Cohort Study. J Invest Surg 2016;29:383-8. [Crossref] [PubMed]
- He G, Zhang D, Gao L, et al. Modified video-assisted technique combined with intraoperative neuromonitoring for preservation of the external branch of the superior laryngeal nerve. Chin J Gen Surg 2019;34:255-6.
- Jiang J, He G, Chu J, et al. Single-incision gasless trans-subclavian endoscopic approach thyroidectomy. Updates Surg 2025;77:175-82. [Crossref (VSports手机版)] [PubMed]
- Thyroid Surgeon Committee of Chinese Medical Doctor Association. Surgical Branch; Thyroid Disease Professional Committee of Chinese Research Hospital Association; Thyroid Surgical Equipment Committee of the Surgical Equipment Branch, China Medical Equipment Association. Expert Consensus on the Protection and Monitoring of the External Branch of the Superior Laryngeal Nerve (EBSLN) during Thyroid and Parathyroid Surgery (2017 Edition). Chinese Journal of Practical Surgery 2017;37:1243-9.
- Sun H, Tian W. Chinese guidelines on intraoperative neuromonitoring in thyroid and parathyroid surgery (2023 edition). Gland Surg 2023;12:1031-49. [Crossref] [PubMed]
- Zhang D, Gao L, He G, et al. Predictors of graft function after parathyroid autotransplantation during thyroid surgery. Head Neck 2018;40:2476-81. [Crossref] [PubMed]
- Cernea CR, Ferraz AR, Nishio S, et al. Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck 1992;14:380-3. [Crossref] [PubMed]
- Friedman M, LoSavio P, Ibrahim H. Superior laryngeal nerve identification and preservation in thyroidectomy. Arch Otolaryngol Head Neck Surg 2002;128:296-303. [VSports注册入口 - Crossref] [PubMed]
- Deniwar A, Kandil E, Randolph G. Electrophysiological neural monitoring of the laryngeal nerves in thyroid surgery: review of the current literature. Gland Surg 2015;4:368-75. [Crossref] [PubMed]
- Barman S, Bhattacharjee A, Mahanta B, et al. Role of Intraoperative Neuromonitoring to Identify External Branch of Superior Laryngeal Nerve During Thyroidectomy. Indian J Otolaryngol Head Neck Surg 2025;77:57-62. [Crossref] [PubMed]
- Bourabaa S, Settaf A. Is identification and dissection of the external laryngeal nerve necessary during thyroidectomy? A prospective study. BMC Surg 2024;24:46. [Crossref] [PubMed]
- Chen H, Xu K, Peng X, et al. Key points for protecting the external branch of the superior laryngeal nerve in open thyroidectomy: A possible exploration technique. Surg Oncol 2024;53:102059. [Crossref] [PubMed]
- Zhou B, Zhai Y, Hei H, et al. The strap intermuscular approach can significantly increase the exposure rate of the external branch of the superior laryngeal nerve during thyroid surgery. Surg Oncol 2020;35:56-61. [Crossref] [PubMed]
- He G, Jiang J, Chu J, et al. Clinical analysis of modified endoscopic total thyroidectomy via gasless unilateral subclavian approach for papillary thyroid carcinoma. Journal of Xian Jiaotong University 2024;1:80-6. (Medical Sciences).
- Zhang D, He G, Chu J, et al. Modified gasless trans-subclavian approach endoscopic lateral neck dissection for treatment of papillary thyroid carcinoma: a series of 31 cases. Chinese Journal of Surgery 2023;61:801-6. [VSports在线直播 - Crossref] [PubMed]
- Berber E, Bernet V, Fahey TJ 3rd, et al. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Li C, Zhang J, Dionigi G, et al. Assessment of different classification systems for predicting the risk of superior laryngeal nerve injury during thyroid surgery: a prospective cohort study. Front Endocrinol (Lausanne) 2023;14:1301838. [Crossref] [PubMed]