V体育2025版 - The significance of implementing the Chinese expert consensus on the prevention and treatment of chyle leakage after neck dissection for thyroid cancer: a single-center retrospective study
Highlight box
Key findings
• The implementation of the 2022 Chinese expert consensus significantly reduced the incidence of chyle leakage from 7. 8% to 1 V体育官网入口. 6% in patients undergoing lateral neck lymph node dissection for papillary thyroid carcinoma (PTC).
What is known and what is new?
• Chyle leakage is a rare but serious complication of neck lymph node dissection, occurring in 2–8% of cases, and can lead to severe outcomes such as electrolyte imbalances and infection VSports在线直播. Conservative management is the first-line approach, with surgical intervention reserved for refractory cases.
• This study provides the first real-world evidence of the effectiveness of the 2022 Chinese expert consensus in reducing chyle leakage incidence V体育2025版. It highlights the importance of standardized surgical techniques, such as meticulous ligation and intraoperative monitoring, as well as the use of local adhesives, in preventing this complication.
What is the implication, and what should change now?
• The findings support the clinical value of the 2022 Chinese expert consensus in improving outcomes for patients undergoing lateral neck lymph node dissection for PTC VSports app下载. Standardized surgical techniques and conservative management strategies are crucial in minimizing chyle leakage and its associated complications.
• The study recommends the widespread adoption of the consensus guidelines, particularly in high-risk patients undergoing left-sided dissections.
Introduction
Chyle leakage represents one of the complications associated with neck lymph node dissection, characterized by a relatively low incidence rate ranging from 2% to 8% VSports手机版. However, it can lead to severe clinical consequences, including electrolyte imbalances, hypoproteinemia, infection, and flap necrosis (1-3). Lymph node metastasis is recognized as one of the most prevalent pathways for the dissemination of papillary thyroid carcinoma (PTC), with approximately 20% of patients presenting with lateral neck lymph node metastasis (4). For this subset of patients, neck lymph node dissection serves as a critical and effective therapeutic intervention.
In an effort to mitigate the incidence of chyle leakage, enhance postoperative management, and standardize the practice of neck lymph node dissection among thyroid surgeons, Chinese experts formulated and released the “Chinese expert consensus on clinical practice of prevention and treatment of chyle leak in neck dissection of thyroid cancer (2022 edition)” in 2022 (5). This consensus document offers comprehensive guidance and recommendations encompassing preoperative preparation, intraoperative preventive strategies, and postoperative identification and management of chyle leakage. Following the dissemination of this consensus, our institution implemented a series of preventive and therapeutic measures aimed at addressing chyle leakage. The present study retrospectively analyzed clinical data from patients who underwent lateral neck lymph node dissection for PTC, comparing outcomes before and after the adoption of the consensus. The primary objective of this investigation was to evaluate the impact of the consensus on the prevention of chyle leakage in this patient population. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-135/rc).
Methods
This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (No. I2025407) and informed consent was taken from all the patients. This retrospective study analyzed cases of patients who underwent lateral neck lymph node dissection for PTC at our institution between May 2020 and December 2023. To minimize variability in surgical outcomes attributable to differences in surgical experience and techniques, all included cases were performed by a single highly experienced thyroid surgeon, Dr. Li Zhiyu. Cases with a previous surgical history of thyroid cancer or severe cardiopulmonary disease were excluded. Beginning in January 2023, our center adopted preventive and therapeutic measures for chyle leakage in accordance with the recommendations outlined in the “Chinese expert consensus on clinical practice of prevention and treatment of chyle leak in neck dissection of thyroid cancer (2022 edition)”.
Surgical procedure
Prior to the implementation of the consensus, the management of lymphatic vessels at the jugular angle in our center primarily involved meticulous and reliable local ligation. In cases where lymphatic vessel leakage was identified, the leakage site was re-ligated or sutured to ensure proper closure.
Following the implementation of the consensus, the operative approach was standardized based on the consensus guidelines, with the following key procedural steps clearly defined: (I) given the histological characteristics of lymphatic vessels, reliable ligation must be performed during the dissection of the venous angle; (II) if lymphatic vessel damage is identified, the leakage site should first be precisely located, and the severed end should be ligated. Alternatively, non-absorbable sutures may be used to suture the surrounding fibrofatty tissue to ensure complete closure; (III) after ligating the damaged lymphatic vessel, a portion of the omohyoid muscle or sternocleidomastoid muscle flap may be utilized to pack and compress the area adjacent to the venous angle; (IV) when deemed necessary, inactivated Pseudomonas aeruginosa solution may be applied to the jugular angle region to promote local tissue adhesion and reduce the risk of postoperative chyle leakage; (V) prior to irrigating the surgical field, the field should be maintained in a clean state, and the anesthesiologist should assist by performing lung inflation for 10–15 seconds to increase intrathoracic pressure, facilitating careful observation for any signs of chyle leakage.
Postoperative prevention and management
The diagnosis of chyle leakage is established based on the following criteria: a progressive increase in postoperative neck drainage volume, a change in the drainage fluid color from serous to milky white, and exacerbation of leakage following oral intake; and/or a triglyceride level in the drainage fluid exceeding 100 mg/dL (6).
Upon confirmation of chyle leakage, non-surgical management is initiated as the first-line approach. This includes the implementation of a low-fat or fat-free diet to reduce chyle production. Maintaining drainage patency and ensuring continuous drainage are critical components of management. Local compression dressing should be applied with precision, typically using 1–2 gauze pads fashioned into a soft ball with a diameter of 3–5 cm, positioned at the surface projection of the venous angle in the supraclavicular fossa. For patients with high-volume leakage (defined as drainage exceeding 1,000 mL/24 hours), fasting combined with parenteral nutrition and somatostatin therapy is recommended. If conservative measures fail to control the leakage, surgical intervention is considered. Following the implementation of the consensus, inactivated Pseudomonas aeruginosa solution may be applied locally to promote tissue adhesion and facilitate fistula closure. In this study, patients were followed up to 1 month after recovery and discharge to determine whether there was recurrence. The median follow-up time was 32 (range, 32–60) days.
Statistical analysis (VSports在线直播)
Descriptive statistics are reported as mean ± standard deviation for normally distributed data, or as median (range) for non-normally distributed data. Comparative analyses between groups were conducted using the chi-square test for categorical variables and the t-test for continuous variables. All statistical analyses were performed using SPSS version 27 software, with a two-sided P value of <0.05 considered statistically significant.
Results
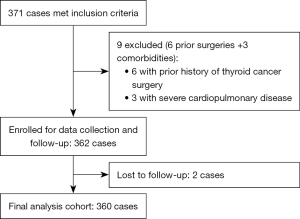
Of 371 initially eligible patients, 9 were excluded (6 with prior thyroid cancer surgery and 3 with severe cardiopulmonary disease). From the remaining 362 cases, 2 were lost to follow-up, resulting in a final analytical cohort of 360 patients (Figure 1). This cohort comprised 231 pre-consensus and 129 post-consensus cases, with comparable baseline characteristics between groups (all P>0.05). The standardized selection process enhanced methodological rigor while controlling for potential confounders. Comparative analyses focused on chyle leakage incidence and management outcomes.
Baseline characteristics
No statistically significant differences were observed between the pre-consensus and post-consensus groups in terms of age (40.4±13.3 vs. 40.7±13.9 years, P=0.27), gender distribution (male proportion: 34.6% vs. 30.2%, P=0.80), body mass index (BMI) (23.9±3.5 vs. 23.5±3.7 kg/m2, P=0.39), surgical extent (left/right/bilateral proportions, P=0.84), tumor (T) stage distribution (T1–4, P=0.52), nodal (N) stage distribution (N0/N1, P=0.38), or operative time (161.3±67.4 vs. 191.1±69.6 min, P=0.38) (Table 1).
Table 1
| Variable | Pre-consensus (n=231) | Post-consensus (n=129) | P value |
|---|---|---|---|
| Age, years | 40.4±13.3 | 40.7±13.9 | 0.27 |
| Gender | 0.80 | ||
| Male | 80 | 39 | |
| Female | 151 | 90 | |
| BMI, kg/m² | 23.9±3.5 | 23.5±3.7 | 0.39 |
| Surgical extent | 0.84 | ||
| Left | 112 | 58 | |
| Right | 95 | 56 | |
| Bilateral | 24 | 15 | |
| T stage | 0.52 | ||
| T1 | 190 | 102 | |
| T2 | 26 | 21 | |
| T3 | 6 | 2 | |
| T4 | 9 | 4 | |
| N stage | 0.38 | ||
| N0 | 30 | 19 | |
| N1 | 201 | 110 | |
| Operative time, min | 161.3±67.4 | 191.1±69.6 | 0.38 |
Data are represented as sample counts or mean ± standard deviation. BMI, body mass index; N, node; T, tumor.
Chyle leakage analysis
Among the study cohort, 39 patients underwent bilateral lateral neck lymph node dissection, resulting in a total of 399 lateral neck lymph node dissections. Chyle leakage was identified in 20 cases (4.8%), with 18 cases (7.8%) occurring in the pre-consensus group and 2 cases (1.6%) in the post-consensus group, demonstrating a statistically significant reduction (P=0.01) (Table 2). Analysis of chyle leakage cases revealed a significantly higher proportion of left-sided lymph node dissections compared to right-sided dissections (80.0% vs. 20.0%, P=0.01). However, no significant association was observed between chyle leakage and IV lymph node positivity (60.0% vs. 70.2%, P=0.35). The maximum postoperative drainage volume in the chyle leakage group was significantly higher than in the non-chyle leakage group (median 325 vs. 90 mL, P<0.01), and the duration of drainage tube retention was also significantly longer in the chyle leakage group (median 13 vs. 1 day, P<0.01).
Table 2
| Variable | Chyle leakage (n=20) | Non-chyle leakage (n=379) | P value |
|---|---|---|---|
| Pre/post consensus | 0.01 | ||
| Pre-consensus | 18 | 237 | |
| Post-consensus | 2 | 142 | |
| Lymph node dissection side | 0.01 | ||
| Left | 16 | 193 | |
| Right | 4 | 186 | |
| IV lymph node | 0.35 | ||
| Positive | 12 | 265 | |
| Negative | 8 | 114 | |
| Max postoperative drainage, mL | 325 [60–1,220] | 90 [10–480] | <0.01 |
| Drainage tube removal time, days | 13 [6–22] | 1 [1–8] | <0.01 |
Data are represented as sample counts or median [range].
Chyle leakage treatment and outcomes (V体育ios版)
All patients diagnosed with chyle leakage were initially managed with conservative treatment, which included continuous drainage, local compression, a fat-free diet, and, in some cases, the application of local adhesives. Conservative management was successful in 16 patients (80%), resulting in resolution of the leakage and eventual removal of the drainage tubes (Figure 2). The remaining 4 patients, who did not respond adequately to fasting, parenteral nutrition, and somatostatin therapy, required surgical intervention, which successfully controlled the leakage and allowed for drainage tube removal. Notably, the use of local adhesives was implemented only after the consensus release and demonstrated efficacy in reducing neck drainage volume. All 4 cases requiring surgical intervention were from the pre-consensus group, whereas both chyle leakage cases in the post-consensus group were successfully managed with conservative measures alone.

Discussion
Chyle leakage is a rare yet clinically significant complication following head and neck surgery, with an incidence rate ranging from 2% to 8% in neck dissection cases (1-3). In this study, 399 lateral neck lymph node dissections were analyzed, revealing an overall chyle leakage rate of 4.8%, which aligns with findings from prior studies. Baker et al. (7) reported that the incidence of chyle leakage following lateral neck lymph node dissection for PTC is significantly higher compared to that for oral squamous cell carcinoma. This discrepancy may be attributed to the greater propensity of thyroid cancer to metastasize to the lower neck lymph nodes (4). To eliminate the confounding effects of varying pathological types on postoperative chyle leakage, this study exclusively included patients diagnosed with PTC.
Furthermore, previous studies have indicated that left-sided lateral neck lymph node dissections are associated with a relatively higher incidence of chyle leakage (8). This study corroborates this finding, with 16 out of 20 chyle leakage cases occurring following left-sided dissections. However, no significant association was observed between IV lymph node positivity and the occurrence of chyle leakage. Previous studies have reported inconsistent results regarding this association (2,3), which may be attributable to differences in the pathological types included across studies. Wang et al. (3), focusing specifically on thyroid cancer, found no significant correlation between IV lymph node positivity and chyle leakage, which was consistent with our study.
The baseline data, including the extent of lateral neck lymph node dissection and tumor stage, demonstrated no significant differences between the pre-consensus and post-consensus groups. Following the implementation of the consensus, the incidence of chyle leakage at our center decreased significantly (1.6% vs. 7.8%, P=0.01), likely due to the identification of high-risk patients and the adoption of more standardized intraoperative dissection techniques at the venous angle. As detailed in the Methods section of this paper, our center consistently employed surgical techniques that emphasize active identification and necessary ligation of the thoracic duct and its branches. Regarding the modified chyle leakage prevention measures implemented after adopting the consensus (compared to our previous protocols), we will now focus our discussion on these key aspects. Drawing on previous research (9), the consensus recommends that prior to irrigating the surgical field, the anesthesiologist should perform lung inflation for 10–15 seconds to increase intrathoracic pressure, facilitating the identification of potential chyle leakage. Roh et al. (1) demonstrated that intraoperative careful observation can detect approximately 50% of chyle leakages, and appropriate ligation or suturing during surgery can prevent postoperative chyle leakage. Since implementing the consensus guidelines in clinical practice, our center has systematically implemented meticulous intraoperative irrigation with thorough inspection and immediate management of suspected chyle leakage prior to irrigating the surgical field. Combined with previous research findings, this modified protocol represents one of the key factors contributing to our observed reduction in postoperative chyle leakage rates. However, as this is a retrospective study, our case records did not systematically document intraoperative findings of chyle leakage. Therefore, this study could not statistically analyze: (I) the differences in intraoperative chyle leakage detection rates before versus after implementation of the Chinese consensus; or (II) the potential correlation between intraoperative findings and subsequent postoperative chyle leakage occurrence. Additionally, based on the findings of Genpeng et al. (10) the intraoperative application of local adhesives has been shown to reduce the incidence of chyle leakage following thyroid cancer surgery and the volume of drainage fluid. In accordance with the consensus recommendations, we prophylactically applied local adhesives, Pseudomonas aeruginosa solution, in high-risk patients, such as those undergoing left-sided lateral neck lymph node dissection or with suspected intraoperative chyle leakage, to mitigate the risk of postoperative chyle leakage. Following implementation of the standardized intraoperative protocol for chyle leakage prevention—including systematic lung inflation testing before irrigation to identify leakage sites, application of Pseudomonas aeruginosa solution, and other corresponding measures—the average maximum postoperative cervical drainage volume significantly decreased to 97 mL (compared to 127 mL prior to protocol implementation, P=0.02). As this comprehensive protocol involves multiple simultaneous interventions, the observed reduction in drainage output reflects the combined efficacy of these integrated measures. The primary objective of this study was to evaluate the collective clinical impact of these multimodal preventive strategies. The relative contribution of each individual measure within this protocol may require further clarification through prospective studies specifically designed to isolate their respective effects.
For the management of chyle leakage, conservative treatment is generally the first-line approach, with surgical intervention reserved for cases refractory to conservative measures. In this study, the majority of chyle leakages (80%) were successfully managed with conservative treatment, which included nutritional support, continuous drainage, somatostatin therapy, local compression dressing, and the application of local adhesives. Patients with chyle leakage are advised to adhere to a low-fat or fat-free diet to reduce chyle production (11,12). Given the substantial loss of water and electrolytes associated with chyle leakage, careful monitoring and supplementation are essential to prevent electrolyte imbalances. For patients with high-volume chyle leakage unresponsive to a fat-free diet, fasting combined with total parenteral nutrition is recommended to minimize intestinal chyle production (13). Continuous drainage not only facilitates the observation of drainage fluid characteristics and eliminates dead space but also aids in monitoring the efficacy of conservative treatment. A previous study suggests that continuous high-negative-pressure suction may enhance the management of chyle leakage (8). In the present study, continuous drainage was consistently employed as the primary treatment for postoperative chyle leakage, both before and after implementation of the consensus. Somatostatin and its analogs, such as octreotide, may reduce chyle production by inhibiting pancreatic and gastrointestinal secretions, lowering hepatic venous pressure, and reducing splanchnic blood flow through endocrine and paracrine pathways, or by directly acting on vascular somatostatin receptors (14). However, the relevant results still remain somewhat controversial and require further randomized controlled studies to fully understand this effect. Local compression dressing is believed to promote the closure of chyle leakage (15), although concerns have been raised regarding the risk of impaired flap perfusion (16). Our center previously introduced the “finger-pressing method” as a local compression technique for postoperative chyle leakage, with favorable outcomes (17). Additionally, the use of Pseudomonas aeruginosa injection as an adhesive for treating chyle leakage following neck lymph node dissection has been reported to yield positive results (18). Through these conservative measures, the majority of chyle leakages can be effectively managed. In this study, the conservative treatment approaches were generally similar before and after implementation of the consensus, with the addition of local adhesive (Pseudomonas aeruginosa solution) application in the post-Consensus period to reduce chyle leakage volume. While these measures contributed to the absence of reoperations for high-output chyle leakage in the post-Consensus cohort (0% vs. 1.6% pre-consensus, P=0.13), this difference did not reach statistical significance. The reduction in reoperations primarily reflects the effectiveness of improved intraoperative preventive measures in decreasing the occurrence of high-volume postoperative chyle leakage, whereas postoperative management strategies mainly serve as salvage therapies. Notably, the proportion of high-output chyle leakage cases requiring reoperation in our study was 20% of all chyle leakage cases, which is consistent with previously reported data (19.9%) (9). However, certain cases, particularly those with high-volume leakage, may not respond adequately to conservative treatment and may require surgical intervention to ligate or suture the fistula. The Chinese consensus provides recommendations on the timing and indications for surgical intervention based on existing literature. For high-volume chyle leakage (defined as continuous drainage exceeding 2,000 mL/day), failure of conservative treatment, or the development of severe complications such as electrolyte imbalances or severe hypoproteinemia, surgical intervention is recommended (5). Furthermore, the consensus recommends performing reoperation under superficial cervical plexus block anesthesia rather than general anesthesia. This approach allows for preoperative consumption of a high-fat diet, which facilitates better intraoperative identification of chyle leakage fistulas. Due to tissue edema in the surgical area, simple suturing of the lymphatic vessel wall may be challenging, and the main lymphatic trunk, along with surrounding tissue, should be sutured together.
There are several limitations in this study. Its retrospective design precludes the control of all potential confounding variables. By focusing exclusively on patients undergoing lateral neck lymph node dissection for PTC, this study eliminated the influence of different pathological types on chyle leakage but also limited the generalizability of the findings to this specific patient population. Additionally, as a single-center study, it did not account for variations in surgical techniques, proficiency, and treatment measures across different institutions, making it difficult to assess the broader impact of the Chinese consensus in diverse clinical settings. As a retrospective study, our case records lacked systematic documentation of intraoperatively identified chyle leakage events. Consequently, this analysis could not evaluate: the detection rates of intraoperative chyle leakage, or its potential correlation with subsequent postoperative leakage development. Future prospective studies should incorporate standardized intraoperative documentation of these findings to better elucidate the individual efficacy of each preventive measure implemented during surgery. Future multicenter prospective studies are warranted to elucidate which preventive and therapeutic measures outlined in the Chinese consensus have a significant impact on chyle leakage.
Conclusions
This study conducted a retrospective comparison of the incidence and management of chyle leakage in patients undergoing lateral neck lymph node dissection for PTC before and after the implementation of the “Chinese expert consensus on clinical practice of prevention and treatment of chyle leak in neck dissection of thyroid cancer (2022 edition)”. The findings demonstrated that the implementation of the consensus—particularly through standardized protocols including pre-irrigation lung inflation testing for intraoperative chyle leakage detection with corresponding management, and the application of Pseudomonas aeruginosa solution—led to a significant reduction in the incidence of chyle leakage within this patient population. These results underscore the critical importance of systematic prevention and management strategies for chyle leakage in patients undergoing lateral neck lymph node dissection for PTC.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-135/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-135/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-135/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-135/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (No. I2025407) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roh JL, Kim DH, Park CI. Prospective identification of chyle leakage in patients undergoing lateral neck dissection for metastatic thyroid cancer. Ann Surg Oncol 2008;15:424-9. [Crossref] [PubMed]
- Ahn D, Sohn JH, Jeong JY. Chyle Fistula After Neck Dissection: An 8-Year, Single-Center, Prospective Study of Incidence, Clinical Features, and Treatment. Ann Surg Oncol 2015;22:S1000-6. [Crossref] [PubMed]
- Wang X, Wang S, Li C, et al. Lymph or Chyle Leak After Neck Dissection in Patients With Thyroid Carcinoma: Results of a Study on 1724 Patients. Am Surg 2022;88:109-14. [Crossref] [PubMed]
- Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007;245:604-10. [Crossref] [PubMed]
- Chinese Research Hospital Association Thyroid Disease Committee. Chinese Thyroid Association CCoSCMDA, Clinical Practical Technology Branch of Chinese Medical Care International Exchange Promotion Association. Chinese expert consensus on clinical practice of prevention and treatment of chyle leak in neck dissection of thyroid cancer (2022 edition). Chinese Journal of Practical Surgery 2022;42:616-20.
- Delaney SW, Shi H, Shokrani A, et al. Management of Chyle Leak after Head and Neck Surgery: Review of Current Treatment Strategies. Int J Otolaryngol 2017;2017:8362874. [Crossref] [PubMed]
- Baker A, Tassone P, Dooley LM, et al. Postoperative Chyle Leak Rate Following Neck Dissection for Squamous Cell Carcinoma Versus Papillary Thyroid Cancer. Laryngoscope 2023;133:2959-64. [Crossref] [PubMed]
- Wu G, Chang X, Xia Y, et al. Prospective randomized trial of high versus low negative pressure suction in management of chyle fistula after neck dissection for metastatic thyroid carcinoma. Head Neck 2012;34:1711-5. [Crossref] [PubMed]
- Park I, Her N, Choe JH, et al. Management of chyle leakage after thyroidectomy, cervical lymph node dissection, in patients with thyroid cancer. Head Neck 2018;40:7-15. [Crossref] [PubMed]
- Genpeng L, Jinen S, Tao W, et al. Intraoperative application of inactivated Pseudomonas aeruginosa in patients undergoing lateral neck dissection for metastatic thyroid cancer: A randomized, parallel group, placebo-controlled trial. Surgery 2020;168:340-6. [Crossref] [PubMed]
- Campisi CC, Boccardo F, Piazza C, et al. Evolution of chylous fistula management after neck dissection. Curr Opin Otolaryngol Head Neck Surg 2013;21:150-6. [Crossref (VSports)] [PubMed]
- Mori Y, Yamashita H, Sato S, et al. Usefulness of preoperative ice cream consumption and novel postoperative drainage management in patients undergoing left-sided neck dissection for thyroid cancer: a nonrandomized prospective study. Surg Today 2024;54:642-50. [Crossref] [PubMed]
- Bibby AC, Maskell NA. Nutritional management in chyle leaks and chylous effusions. Br J Community Nurs 2014;Suppl Nutrition:S6-8.
- Coşkun A, Yildirim M. Somatostatin in medical management of chyle fistula after neck dissection for papillary thyroid carcinoma. Am J Otolaryngol 2010;31:395-6. [Crossref] [PubMed]
- Nussenbaum B, Liu JH, Sinard RJ. Systematic management of chyle fistula: the Southwestern experience and review of the literature. Otolaryngol Head Neck Surg 2000;122:31-8. [Crossref] [PubMed]
- de Gier HH, Balm AJ, Bruning PF, et al. Systematic approach to the treatment of chylous leakage after neck dissection. Head Neck 1996;18:347-51. ["VSports在线直播" Crossref] [PubMed]
- Xiang D, Liu Z, Yang T, et al. Finger-pressing: a simple and efficient way to stop chyle leak post neck dissection. Endocrine 2020;67:374-8. [Crossref] [PubMed]
- Chen Q, Chen Y, Su A, et al. Ultrasound-guided percutaneous injection of Pseudomonas aeruginosa-mannose sensitive hemagglutinin for treatment of chyle fistula following neck dissection: Two case reports. Medicine (Baltimore) 2020;99:e18816. [Crossref] [PubMed]